Overview of atrial fibrillation
INTRODUCTION — Atrial fibrillation (AF) is the most common cardiac arrhythmia that has the following electrocardiographic characteristics.
- The RR intervals follow no repetitive pattern—they have been labeled as “irregularly irregular.”
- While electrical activity suggestive of P waves is seen in some leads, there are no distinct P waves. Thus, even when an atrial cycle length (the interval between two atrial activations or the P-P interval) can be defined, it is not regular and often less than 200 milliseconds (translating to an atrial rate greater than 300 beats per minute).
AF can have adverse consequences related to a reduction in cardiac output and to atrial and atrial appendage thrombus formation In addition affected patients may be at increased risk for mortality.
PATHOGENESIS — Irrespective of the underlying risk factor(s), changes in the electrophysiology of the atrial myocardium are likely important. The pathophysiology of atrial fibrillation (AF) is discussed in detail elsewhere.
CLASSIFICATION
General classification — Historically, the terms acute and chronic AF were used to describe the temporal nature of a patient’s atrial fibrillation (AF). These two terms have been replaced with the following classification schema proposed by the American College of Cardiology/American Heart Association and the European Society of Cardiology
- First detected or diagnosed AF, independent of the duration of AF or the presence or absence of symptoms.
- Paroxysmal (ie, self-terminating or intermittent) AF — Paroxysmal AF is defined as recurrent AF (≥2 episodes) that terminates spontaneously in seven days or less, usually less than 24 hours.
- Persistent AF — Persistent AF is defined as AF that fails to self-terminate within seven days. Episodes often require pharmacologic or electrical cardioversion to restore sinus rhythm. While a patient who has had persistent AF can have later episodes of paroxysmal AF, AF is generally considered a progressive disease. In individuals with paroxysmal AF, progression to persistent and permanent AF occur in >50 percent beyond 10 years despite antiarrhythmic therapy
- Long-standing persistent AF, which refers to persistent AF that has lasted for one year or more.
- Permanent AF — Permanent AF is a term used to identify individuals with persistent atrial fibrillation where a decision has been made to no longer pursue a rhythm control strategy
This classification applies to recurrent episodes of AF that last more than 30 seconds and that are unrelated to a reversible cause. If the AF is secondary to cardiac surgery, pericarditis, myocardial infarction (MI), hyperthyroidism, pulmonary embolism, pulmonary disease, or other reversible causes, therapy is directed toward the underlying disease as well as the AF.
Lone AF — The term lone AF is less often used than in the past and was not included in the ACC/AHA/ESC guidelines discussed above. Lone AF has generally referred to patients with paroxysmal, persistent, or permanent AF who have no structural heart disease. It has primarily been applied to patients ≤60 years of age and identifies a group of individuals at lowest risk of complications associated with AF, including embolization. By definition, such patients have a CHADS2 score of “0”
The following are characteristics of this low-risk population:
- Depending in part upon the population studied and the definition used, lone AF accounts for less than 15 to as many as 30 percent of cases of permanent AF and 25 to 45 percent of cases of paroxysmal A
- Affected patients are younger than those with structural heart disease and are often male
- Patients with lone AF are often symptomatic and associate certain triggers with episodes of AF. In a series of 181 patients (94 percent of whom had paroxysmal AF), the following triggers were reported (percent): sleeping (44), exercise (36), alcohol (36), eating (34)
- Patients with exercise-related AF could have it as a consequence of high catechol levels during exercise or during the period of high vagal tone after exercise.
- In a study of 110 individuals with lone AF, a family history of AF was present in up to 38 percent
- Using Danish national registers, over 9000 individuals with lone AF were identified. The incidence rate ratios (IRR) for lone AF given an affected first- or second-degree relative were significantly increased at 3.48 and 1.64, respectively For individuals less than 40 years of age with an affected first-degree with age onset also less than 40 years, the IRR was 5.42.
Familial aggregation in lone AF is common, as demonstrated in the following two studies:
Recurrent AF — Continuous monitoring studies have shown that approximately 90 percent of patients have recurrent episodes of AF. However, up to 90 percent of episodes are not recognized by the patient , and asymptomatic episodes lasting more than 48 hours are not uncommon, occurring in 17 percent of patients in a report using continuous monitoring. The latter study also showed that 40 percent of patients had episodes of AF-like symptoms in the absence of AF.
Subclinical AF — Subclinical AF, which is a term that is used uncommonly by cardiologists who specialize in arrhythmias, is defined as AF detected (with any monitoring technique) in asymptomatic individuals without a prior diagnosis. Most of these individuals will have PAF. This issue is discussed in detail elsewhere.
The relationship between subclinical AF and cryptogenic stroke is discussed elsewhere.
EVALUATION — The history, physical examination, and specific laboratory and cardiologic testing are all part of the evaluation of the patient with atrial fibrillation (AF).
History and physical examination — Not all patients with AF are symptomatic. Among those that are, symptoms associated with AF are variable and the history should focus on obtaining the following information:
- A description of the symptoms: onset or date of discovery, the frequency and duration, severity, and qualitative characteristics.Typical symptoms include palpitations, tachycardia, fatigue, weakness, dizziness, lightheadedness, reduced exercise capacity, increased urination, or mild dyspnea. More severe symptoms include dyspnea at rest, angina, presyncope, or infrequently, syncope. In addition, some patients present with an embolic event or the insidious onset of right-sided heart failure (as manifested by peripheral edema, weight gain, and ascites).
- Precipitating causes: exercise, emotion, or alcohol.
- The presence of the following disease associations: cardiovascular or cerebrovascular disease, diabetes, hypertension, chronic obstructive pulmonary disease, or potentially reversible causes (eg, hyperthyroidism, excessive alcohol ingestion).
- A complete examination of the cardiovascular system should be performed in all individuals with newly diagnosed AF and in those with a change in symptom status. Abnormal findings may inform health care providers about either contributing factors for (eg, murmur of mitral stenosis) or the impact of (eg, evidence of heart failure) AF.
Electrocardiogram — The electrocardiogram (ECG) is used to verify the presence of AF and is necessary to make the diagnosis. There are a number of potential pitfalls in the electrocardiographic diagnosis of AF. Errors in the diagnosis of AF are especially common with computerized ECG interpretation and in patients who are continuously or intermittently paced. Hence, it is important that the ECG rhythm reported automatically by the machine is interpreted by a skilled reader.
The ECG should also be evaluated for the following information:
Additional testing — Exercise testing is reasonable for patients with signs or symptoms of ischemic heart disease. It is also useful to help guide pharmacotherapy for AF as some antiarrhythmic medications are contraindicated in patients with coronary artery disease.
Holter monitoring or event recorders are used to identify the arrhythmia if it is intermittent and not captured on routine electrocardiography and assess overall ventricular response rates, especially in individuals where a rate control strategy has been chosen.
Clinical or subclinical hyperthyroidism is present in less than 5 percent of patients with AF. A thyroid-stimulating hormone (TSH) should be obtained in all patients with a first episode of AF.
Other important baseline tests include a complete blood count, a serum creatinine, an analysis for proteinuria, and a test for diabetes mellitus.
A rate control strategy generally uses drugs that slow conduction across the atrioventricular (AV) node, such as beta blockers, non-dihydropyridine calcium channel blockers, or digoxin.
Current data suggest that rhythm and rate control strategies are associated with similar rates of mortality and serious morbidity, such as embolic risk. In addition, assessments of quality of life have not shown significant differences between the two in many studies.
The decision to adopt a rhythm or rate control strategy is often dictated by the (1) presence of symptoms associated with atrial fibrillation and/or (2) presence of diminutions in left ventricular systolic function thought secondary to the arrhythmia.
The methods to achieve either rate or rhythm control are discussed in detail elsewhere.
Other indications for hospitalization are discussed separately.
In a post hoc analysis of the Women’s Health Study of 34,772 women with a median age of 53 who were free of AF, about three percent developed AF at a median follow-up of 15.4 years. New onset AF was associated with a significantly increased adjusted risk of all-cause, cardiovascular, and non-cardiovascular mortality (hazard ratios [HR] 2.14, 95% CI 1.64-2.77, 4.18, 95% CI 2.69-6.51, and 1.66, 95% CI 1.19-2.30 respectively). Adjustment for nonfatal cardiovascular events, such as myocardial infarction, stroke or heart failure, lowered these risks but incident AF remained significantly associated with all types of mortality (HR 1.7, 2.57, and 1.42 respectively).
The coexistence of cardiovascular disease and chronic AF worsens the patient's prognosis, doubling the cardiovascular mortality:
In addition, in an observational study of over 20,000 individuals in two cohorts, incident AF was associated with an increased risk of sudden cardiac death (hazard ratio 2.47, 95% CI 1.95-3.13) as well as non-sudden cardiac death (hazard ratio 2.98, 95% CI 2.52-3.53). This study reconfirms that AF is associated with increased all-cause mortality (with death often attributable to events related to coronary artery disease and stroke) and it advances our knowledge in that it demonstrates that there is a proportional increase in sudden death as well.
None of these nonrandomized observations proves that AF directly causes an increase in mortality, since they cannot distinguish this possibility from AF being a marker of a confounding factor or factors that affect survival.
The role of evaluating patients with cryptogenic stroke for AF is discussed separately.
- Markers of nonelectrical cardiac disease, such as left ventricular hypertrophy (possible hypertension) or Q waves (possible coronary artery disease)
- Markers of electrical heart disease, such as delta wave or short PR interval (preexcitation) or bundle branch block (conduction system disease)
- The QT interval (to identify the potential risk of antiarrhythmic therapy).
Echocardiogram — The transthoracic echocardiogram (TTE) is performed to evaluate the size of the right and left atria and the size and function of the right and left ventricles; to detect possible valvular heart disease, left ventricular hypertrophy, and pericardial disease; and to assess peak right ventricular pressure.
The TTE may also identify left atrial thrombus, although the sensitivity is low. Transesophageal echocardiography is much more sensitive for identifying thrombi in the left atrium or left atrial appendage and can be used to determine the need for three to four weeks of anticoagulation prior to any attempt at pharmacologic or electrical cardioversion.Additional testing — Exercise testing is reasonable for patients with signs or symptoms of ischemic heart disease. It is also useful to help guide pharmacotherapy for AF as some antiarrhythmic medications are contraindicated in patients with coronary artery disease.
Holter monitoring or event recorders are used to identify the arrhythmia if it is intermittent and not captured on routine electrocardiography and assess overall ventricular response rates, especially in individuals where a rate control strategy has been chosen.
Clinical or subclinical hyperthyroidism is present in less than 5 percent of patients with AF. A thyroid-stimulating hormone (TSH) should be obtained in all patients with a first episode of AF.
Other important baseline tests include a complete blood count, a serum creatinine, an analysis for proteinuria, and a test for diabetes mellitus.
TREATMENT ISSUES — Health care providers are presented with two broad types of patients with atrial fibrillation (AF): those with newly diagnosed AF and those who have been previously diagnosed and managed. Care of the former includes decisions regarding the need for anticoagulation and the choice between rate or rhythm control strategies. For patients with established diagnosis, periodic assessment of the adequacy of treatment is necessary.
New onset AF — Most patients with new onset (ie, first detected or diagnosed) AF present with symptoms related to the arrhythmia. Except for embolization, the symptoms associated with new onset AF are primarily due to a rapid ventricular response. Thus, many patients have dramatic improvement in their sense of well being when the ventricular rate is slowed.
There are two broad management issues that must be addressed early in patients with new onset AF: the prevention of systemic embolization and the choice between a rhythm or rate control strategy, both of which improve symptoms. These issues will be addressed briefly here. More detailed discussions are found elsewhere.
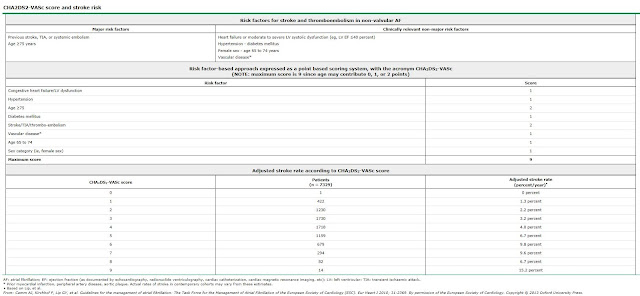
Prevention of systemic embolization — Every patient with AF should be evaluated for the need of antithrombotic therapy to prevent systemic embolization. This has traditionally been accomplished by the application of the CHADS2 risk score. Modifications of this scoring system have resulted in the CHA2DS2-VASc score, which is gaining wider acceptance. Patients who may require antithrombotic therapy include those in whom cardioversion to sinus rhythm is being considered (short-term anticoagulation) and those who meet criteria for chronic anticoagulation. All patients whose risk of embolization exceeds the risk of bleeding are candidates for long-term antithrombotic therapy. These issues are discussed in detail elsewhere.
Rate versus rhythm control — Most patients who present with AF will require slowing of the ventricular rate to improve symptoms.
Once sinus rhythm is achieved, a decision regarding the long-term approach to the management of the rhythm disturbance (rhythm versus rate control) should be made. A rhythm control strategy uses either antiarrhythmic drug therapy, percutaneous catheter ablation, and/or a surgical procedure. Electrical cardioversion may be necessary prior to an attempt to maintain sinus rhythm. Rate slowing drugs are generally started before rhythm control and continued in many patients who remain in sinus rhythm (in the event of return to AF). A rate control strategy generally uses drugs that slow conduction across the atrioventricular (AV) node, such as beta blockers, non-dihydropyridine calcium channel blockers, or digoxin.
Current data suggest that rhythm and rate control strategies are associated with similar rates of mortality and serious morbidity, such as embolic risk. In addition, assessments of quality of life have not shown significant differences between the two in many studies.
The decision to adopt a rhythm or rate control strategy is often dictated by the (1) presence of symptoms associated with atrial fibrillation and/or (2) presence of diminutions in left ventricular systolic function thought secondary to the arrhythmia.
The methods to achieve either rate or rhythm control are discussed in detail elsewhere.
Hospitalization — Some patients with AF may require care at an acute-care facility or an inpatient unit of a hospital. Common indications for care at one or both of these facilities include:
- Management of heart failure or hypotension after control of the rate or rhythm
- Initiation of antiarrhythmic drug therapy
- Treatment of an associated medical problem, which is often the reason for the arrhythmia. Examples include the treatment of hypertension, infection, thyroid storm, exacerbation of chronic obstructive pulmonary disease (COPD), pulmonary embolism, persistent myocardial ischemia, or acute pericarditis.
Other indications for hospitalization are discussed separately.
Paroxysmal, persistent, longstanding persistent, or permanent AF — Patients with paroxysmal, persistent, longstanding persistent, or permanent AF will need periodic care as well as occasional urgent evaluation during the natural history of their disease.
We suggest routine follow-up every twelve months in stable patients and sooner if there are changes in symptoms. Some of our experts see patients on high risk antiarrhythmic therapy, such as dofetilide or sotalol, every six months.
Routine care — From time to time, patients should be monitored for the following:
- Efficacy and safety of antithrombotic therapy (International normalized ratio for patients on warfarin and creatinine clearance for patients on dabigatran)
- Functional status, including change in symptoms (history)
- Efficacy and safety of antiarrhythmic drug therapy (electrocardiogram [ECG], assessment of renal and hepatic function, and perhaps other tests)
- Efficacy of rate control (history, ECG, and perhaps extended Holter monitoring)
Urgent care — Urgent care is necessary in patients who present with symptoms or signs of symptomatic AF.
In addition to evaluating the efficacy of rate or rhythm control, the health care provider many need to evaluate and manage changes in the symptoms and signs of coronary artery disease or heart failure.
LONG-TERM OUTCOME — Atrial fibrillation (AF) is an independent risk factor for mortality across a wide age range and in both men and women. However, we and others believe the evidence is insufficient to label AF as causal. The following studies illustrate the range of risk:
- In a secondary analysis of the randomized controlled AFFIRM trial of rhythm versus rate control in AF, the presence of sinus rhythm was associated with a significant reduction in mortality (hazard ratio 0.53). A similar benefit from being in sinus rhythm (relative risk 0.44) was noted in the DIAMOND trial that compared dofetilide to placebo in patients with reduced left ventricular function.
- In a retrospective observational study of 272,186 patients with incidental AF at the time of hospitalization and 544,344 matched AF free controls, the adjusted relative risk of death for women and men <65 years was 2.15 and 1.76 (respectively), 65 to 74 years 1.72 and 1.36, and 75-85 years 1.44 and 1.24. All values were statistically significant.
- In a report from the Framingham Heart Study in which 621 subjects between the ages of 55 and 94 who developed AF were compared to those who did not. AF almost doubled the risk of death in both men and women. After adjustment for the pre-existing cardiovascular diseases with which AF was associated, AF was still associated with a significantly increased risk of death (odds ratio 1.9 for women and 1.5 for men). Both heart failure (HF) and stroke contributed to the excess mortality.
- In a 20-year follow-up of over 15,000 men and women between the ages of 45 and 64 in which 47 women and 53 men had AF on a single electrocardiogram (ECG) at baseline, the presence of AF was associated with a marked increase in the risk of a cardiovascular event (death or hospitalization) (89 versus 27 percent in women and 66 versus 45 percent in men) and was a significant independent predictor of all-cause mortality (relative risk 2.2 in women and 1.5 in men).
In a post hoc analysis of the Women’s Health Study of 34,772 women with a median age of 53 who were free of AF, about three percent developed AF at a median follow-up of 15.4 years. New onset AF was associated with a significantly increased adjusted risk of all-cause, cardiovascular, and non-cardiovascular mortality (hazard ratios [HR] 2.14, 95% CI 1.64-2.77, 4.18, 95% CI 2.69-6.51, and 1.66, 95% CI 1.19-2.30 respectively). Adjustment for nonfatal cardiovascular events, such as myocardial infarction, stroke or heart failure, lowered these risks but incident AF remained significantly associated with all types of mortality (HR 1.7, 2.57, and 1.42 respectively).
The coexistence of cardiovascular disease and chronic AF worsens the patient's prognosis, doubling the cardiovascular mortality:
- In patients with a recent myocardial infarction (MI), the development of AF increases mortality. This effect is primarily due to associated risk factors, such as HF and cardiogenic shock, not AF itself.
- The effect of AF in the setting of HF is less clear, since published studies have yielded conflicting results and any effect of AF to increase mortality may have diminished with better treatment of HF.
In addition, in an observational study of over 20,000 individuals in two cohorts, incident AF was associated with an increased risk of sudden cardiac death (hazard ratio 2.47, 95% CI 1.95-3.13) as well as non-sudden cardiac death (hazard ratio 2.98, 95% CI 2.52-3.53). This study reconfirms that AF is associated with increased all-cause mortality (with death often attributable to events related to coronary artery disease and stroke) and it advances our knowledge in that it demonstrates that there is a proportional increase in sudden death as well.
None of these nonrandomized observations proves that AF directly causes an increase in mortality, since they cannot distinguish this possibility from AF being a marker of a confounding factor or factors that affect survival.
SCREENING — Despite the known increase in morbidity, such as stroke, and mortality in patients with atrial fibrillation (AF), the issues of how or whether to screen for AF have not been well studied. We do not recommend screening asymptomatic patients for AF. Patients with an irregular pulse at the time of a physical examination should have an electrocardiogram (ECG) performed to determine its cause.
In a multicenter, cluster, randomized trial that included over 14,000 patients, 50 primary care sites were randomly assigned to intervention or control practices (usual care). Within the intervention practices, patients were randomly assigned to a systematic screening arm (invitation for an ECG) or an opportunistic arm (routine pulse taking and ECG only for irregular pulse). As expected, both systematic and opportunistic screening had higher rates of detection of AF than usual care (odds ratios 1.57, 95% CI 1.08-2.26 and 1.58, 95% CI 1.10-2.29). A 2013 systematic review identified this as the only relevant study.The role of evaluating patients with cryptogenic stroke for AF is discussed separately.
INFORMATION FOR PATIENTS — UpToDate offers two types of patient education materials, “The Basics” and “Beyond the Basics.” The Basics patient education pieces are written in plain language, at the 5th to 6th grade reading level, and they answer the four or five key questions a patient might have about a given condition. These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the 10th to 12th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon.
SUMMARY — The following are essential points addressed in this topic:
- Atrial fibrillation (AF) is the most common cardiac arrhythmia that can have adverse consequences related to a reduction in cardiac output (symptoms) and to atrial and atrial appendage thrombus formation (stroke and peripheral embolization). In addition, affected patients may be at increased risk for mortality.
- Hypertensive heart disease and coronary heart disease are the most common underlying disorders in developed countries associated with atrial fibrillation.
- Patients are classified as having new onset, paroxysmal, persistent, longstanding persistent, or permanent AF.
- Essential information from the patient’s history, physical examination, electrocardiogram, and a transthoracic echocardiogram should be obtained at the time of diagnosis and periodically during the course of the disease. Additional laboratory testing, such as thyroid stimulating hormone assay, may be necessary.
- The two principal management decisions for patients are:
- Does the patient need long-term antithrombotic therapy? All patients whose risk of embolization exceeds the risk of bleeding are candidates for such therapy.
- Should the patient be managed with either a rate or a rhythm control strategy? This should be determined based on severity of symptoms, presence of structural heart disease, adequacy of rate control during episodes of atrial fibrillation, and the patient’s preference for using antiarrhythmic drug therapy or undergoing ablation-based interventions.
- In the absence of a reversible precipitant, AF is typically recurrent.




No hay comentarios:
Publicar un comentario